Elimite
"Buy elimite 30 gm line, skin care forum."
By: Jay Graham PhD, MBA, MPH
- Assistant Professor in Residence, Environmental Health Sciences

https://publichealth.berkeley.edu/people/jay-graham/
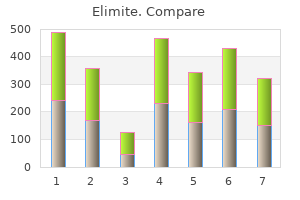
Many patients who do not seek regular dental care will seek treatment when the condition becomes painful or if they are concerned about "bleeding gums skin care 2 in 1 4d motion discount elimite 30gm mastercard. The dentist or hygienist should debride affected areas to remove plaque and calculus acne 5 days before period order elimite 30 gm on line. If necessary, local anesthetic can be used to make the patient more comfortable during this process. Other disease control procedures, such as simple restorations to control caries and endodontic therapy, can be provided during pregnancy, ideally during the second trimester. Elective definitive care, such as crowns, fixed partial dentures, implants, and preprosthetic surgery, should be postponed until after the baby is born. Diabetes Diabetes is a relatively common disease affecting approximately 14 million people in the United States. The number of patients with type 2 diabetes has tripled in the last 30 years and is believed to be associated with an increase in obesity for American adults. The dentist should make note of any medications the patient is taking and be aware of any side effects because several oral hypoglycemics can have an effect on the oral cavity. The level of metabolic control attained by the patient should be assessed from both an overall and a same-day perspective. Most diabetics can accurately assess their level of control on a long-term and short-term basis. At the beginning of each appointment, the dentist should ask the diabetic patient how he or she is feeling, whether food has been eaten that day, and whether insulin or oral hypoglycemic medications have been taken according to instructions. All diabetic patients should make regular visits to the physician and have periodic monitoring of blood sugar levels. The insulin-dependent patient should be questioned about the usual levels of blood glucose maintained and the frequency of blood testing for glucose. Any reported emergency visits for hyperglycemia or hypoglycemia should be documented in the record. Lastly, when reviewing the health questionnaire with the patient, the practitioner should learn whether the patient suffers from any of the other conditions frequently seen in the diabetic patient, such as kidney, cardiovascular, or peripheral vascular diseases. Wellcontrolled diabetics should be advised to eat normal meals before appointments and should be scheduled mid- Figure 5-3 this 20-year-old woman complained of sore gums, was 3 months pregnant, and had pregnancy gingivitis. The patient had poor oral hygiene and the gingiva was inflamed, especially in the mandibular arch. With improved oral hygiene and periodontal treatment, the condition improved and eventually disappeared. Early signs and symptoms of hypoglycemia include hunger, weakness, trembling, pallor, and a rapid heart rate (tachycardia). Because eating regular meals is an important part of glycemic control, especially for the insulin-dependent diabetic, the patient may need to adjust the insulin dosage if he or she will be unable to return to a regular eating schedule immediately after a dental procedure. Some diabetic patients may have a greater incidence of periodontal disease, dental caries, missing teeth, xerostomia, and fungal infections. In addition, they may be more likely to suffer such adverse outcomes after treatment as delayed healing or infection. Diabetic patients may need more frequent periodontal maintenance visits and should be encouraged to maintain a noncariogenic diet and a high level of oral hygiene. Oral Health and the Diabetic Patient Based on the clinical observations of dentists, diabetic patients have traditionally been thought to be more susceptible to oral diseases, such as periodontal disease and dental caries. Most dentists have been taught that diabetic patients may heal poorly and are at increased risk for bacterial and fungal infections. Diabetic patients have been characterized as having a higher incidence of xerostomia and such orofacial pain complaints as burning mouth. In addition, the assumption has been made that physiologic changes associated with diabetes may predispose the diabetic patient to certain dental diseases. For example, a hyperglycemic patient could be expected to have high levels of glucose in gingival crevicular fluid, perhaps leading to a greater incidence of dental caries. These views seem plausible and appear to have been supported by clinical observations. In the past decade, several controlled studies have compared the incidence of certain oral diseases and problems in diabetic patients with incidence in persons who do not have diabetes.
The Importance of Functional and Behavioral Issues Behavioral issues can have an impact on planning dental treatment for any patient acne treatment during pregnancy buy 30gm elimite fast delivery. Patients who are not diligent with their oral self care are more likely to experience the ravages of caries skin care 40 plus buy discount elimite 30 gm line, periodontal disease, and other oral health problems. Patients who are motivationally impaired may require a wide array of special management techniques as discussed in Chapter 17. For the patient with special needs, however, behavioral problems often go far beyond the challenge of finding a means to motivate the patient to be more diligent with oral home care. The patient with special needs may not be able to open his or her mouth, or respond to simple commands, or be oriented to person, place, and time. Some important functional and behavioral questions that must be addressed in the process of developing the treatment plan include the following: · How well was the patient able to cooperate for the radiographic and clinical examinations? How interested is the caregiver in improving the oral health condition of the patient? Behavioral issues can severely limit both the scope and nature of the treatment that can be provided on an outpatient basis. In most cases, the most basic behavioral concern is whether the patient can cooperate for the dental treat- ment. Closely linked with this concern is the corollary question as to whether the patient may require or benefit from some form of sedation or general anesthesia. If, for instance, a patient is resistive and actively uncooperative, then it would be expected that only minimally invasive dental treatment and simple restorative procedures could be performed without sedation. If a patient is passively uncooperative, then it may be possible to provide a full range of treatment with only minimal oral sedation. If the patient is actively uncooperative and the treatment objectives include definitive restorative procedures that necessitate generating diagnostic casts and complete mouth radiographic images, then general anesthesia is usually warranted. The following section briefly summarizes the indications for the various forms of sedation (see also Chapter 13 for more detail. Although it may include behavioral therapies, such as desensitization therapy, relaxation therapy, or hypnosis, its essence is the "sedative" effect that is provided by trust and confidence in the dental team by the patient. The efficiency of most forms of sedation is dependent on the level of iatrosedation the patient experiences. If the patient trusts the dental team and feels emotionally supported and listened to , other forms of sedation will work more efficiently. Nitrous Oxide and Oxygen Analgesia this is a very efficient form of analgesia, but to be used successfully the patient must be able to breathe normally through the nose piece. If the patient is unable or unwilling to be cooperative, allowing nitrous oxide to escape around the mask, or if he or she persists in mouth breathing or talking, then the staff and dentist will be inhaling the nitrous oxide and the effectiveness on the patient will be greatly reduced. There are documented environmental risks for the dental team with this medication, most notably obstetric and reproductive complications. In extremely fearful or agitated patients, however, the dosage required to effectively sedate the patient may be so high that anesthetic risks (unconsciousness or fatal overdose) are not acceptable. Several protocols are available 250 Planning Treatment for Patients With Special Needs for the oral conscious sedation technique. These range from simple anxiolysis to incrementally administered oral sedatives to achieve a desired effect. Airway protection and management are of paramount importance with the use of any pharmacologic sedation. If general dentistry is planned, however, great caution must be observed to protect the airway from particulate matter. Also, completing all treatment in a timely and safe manner can be quite challenging with this modality if many teeth are to be restored, extracted, or treated endodontically. General Anesthesia the decision to place the patient under general anesthesia for general dental care takes into account both the preoperative diagnostic and treatment needs and the postoperative goals. If a comprehensive examination, scaling and root planing, restorations, extractions, etc. A recent physical examination, consent (also called an operative permit in the hospital setting), and anesthesia consultation must occur preoperatively.
Buy cheap elimite 30 gm line. TULA Probiotic Skin Care Deep Wrinkle Serum 1oz on QVC.
Patients who wear an occlusal guard may need an occlusal adjustment or less commonly a reline of the appliance skincarerx generic elimite 30gm online. These procedures can normally be accommodated at the periodic visit if the patient remembers to bring the guard to the appointment acne breakout buy 30gm elimite with visa. If an occlusal guard has completely fractured, it may be best to remake it rather than to try to repair it. Progress Note Documentation of the periodic visit should be recorded in the progress notes in the patient record. If the next visit is for a restorative procedure, the note should include the tooth numbers, surfaces, the material and procedure planned, and evidence of patient consent. In an effort to generate the progress note efficiently and still cover all elements in an appropriately detailed manner, many practitioners are now developing electronic progress notes. Software designed for the purpose creates progress notes characterized by clarity, consistency, legibility, and professional appearance. Some have a skeleton outline, and narrative entries are made electronically with a word processor using the same language and format as with a conventional hand-written chart entry. Others have rather complete and detailed narrative already included, and the provider fills in critical blanks with options from appropriate pull down menus. All of these features can provide considerable time savings compared with the conventional handwritten record. It is expected that as software programs become more available and as the significant benefits of the electronic patient record are more widely appreciated, the use of electronic progress notes for periodic visits and for all dental treatment visits will become standard practice in most dental settings. Health history update-Program recalls the existing health and medication histories; prompts for changes in medications or medical conditions and status. Decision support software can analyze for systemic contraindications and modifications to dental treatment, flag Alerts, and summarize possible drug interactions. Vital signs-Trigger Alert when patient-specific threshold is crossed; note progressive trends over time. Available radiographs-Recalls radiographic log; flag indicates radiographs overdue (standard may be individual for the patient or universal selection criteria). Extraoral and intraoral examination-Recalls previous lesions; queries for new findings; if new findings present, selection menu includes options for location, size, shape, color, consistency, surface characteristics, borders; decision support software can suggest possible differential diagnosis. Periodontal examination · Gingiva-Selection menu prompts: color, density, sites, and depth of inflammation · Pockets-Recorded on odontographic record and changes graphed · Furcas, mucogingival defects, and other clinical abnormalities-Recorded on odontographic record · Bone loss and bony defects-Program prompts for significant positive or negative findings and records 6. Endodontic/periapical pathology-Program queries for significant positive and negative findings (decision support system can render a diagnosis) and records Courtesy Dr. Dental abnormalities-Program queries for significant positive and negative findings and records: · Missing teeth · Caries, fractures, cervical notching · Defective restorations · Others as specified by the practitioner Diagnosis-List generated by the dentist after review of all findings; decision support software can suggest a list of possible conditions or problems. Treatment-Established template provides a starting point; deletions are made online; additions are prompted by a selection menu and can be added online. Plan-Selection menu prompts type of visit (periodic, episodic, surgical, endodontic, periodontic, orthodontic/occlusal, restorative, or other) and interval; details and notes added online. Based on the above information, the computer then generates a comprehensive progress note. Collateral programs can also generate appropriate patient-specific instructional materials. Inclusion of the maintenance phase and its periodic visits in the treatment plan ensures continuity of care for the patient, and a higher quality of record keeping for the practice. The In Clinical Practice box features tips for developing an effective maintenance program. The benefits of a well-established maintenance program to the patient, dentist, and practice are significant. In Clinical Practice Tips for Developing an Effective Maintenance Care Program in Private Practice · Develop a philosophy for your maintenance program. Include all items that should be evaluated, treated, and/or reassessed at future visits. For many, a caregiver must play a central role in taking care of their daily needs. Patients with special care needs provide the dental team with unusual and significant challenges in both planning and delivering dental treatment. Such patients deserve optimal care that is consistent with their dental treatment goals and with their cognitive and physical capacity to maintain a healthy oral condition.
If financial issues are raised too early or insensitively skin care 50th and france order elimite 30 gm with amex, the patient may perceive the queries as an intrusion into his or her private life and conclude that the dentist is "after my money acne vs rosacea purchase 30 gm elimite with amex. Ethics in Dentistry When patients are inconsistent in their own oral health care, erratic in keeping appointments, routinely tardy, or rude to staff, they may be labeled as "difficult," "noncompliant," or "hateful. Healthy professional relationships require mutual effort on the part of the clinician and the patient. Rather than blaming the "difficult patient," it can be valuable to explore why the relationship between dentist and patient is difficult in this particular case. Nisselle1 describes, for example, sharing responsibility for "difficult patients" with a practice partner and finding that some of the patients he perceived as difficult worked very well with his partner and vice versa. When a dentist-patient relationship is perceived as difficult, the clinician should try to identify the underlying reason or source of the difficulty. Once the clinician is able to pinpoint the problem, the issue can be addressed directly with the patient. Resolving difficult clinical relationships requires time and commitment from both dentist and patient. Clear documentation of discussions with the patient may help the dentist support a decision to discontinue a clinical relationship in the event that these efforts fail. Nisselle P: Difficult doctor-patient relationships, Aust Fam Phys 29(1):47-49, 2000. This is not, however, a guarantee that those efforts will be successful because that same patient has complete freedom to accept or reject the rationale and may choose to do so on strictly intellectual grounds. The patient also may choose to reject it because other self-actualizing concepts are more appealing or take precedence. Some environmental factors, such as job stress, can be altered, whereas others realistically cannot. When psychological barriers to change are not significant and when the patient has a positive sense of self-worth, the potential for eliminating deleterious behaviors and promoting positive ones is good. With time, and a professional and supportive approach, these patients may accept the responsibility to change. When these issues are dealt with effectively, educating the patient about the benefits of dental treatment is much easier. The motivationally impaired patient often has poor oral home care, creating an unfavorable environment for the long-term success of any treatment. How much they absorb and how effectively they implement that instruction varies, however. With the motivationally impaired patient, a routine impersonal approach to oral physiotherapy instruction is unlikely to succeed. A compassionate, thoughtful, and patientspecific approach to educating the patient regarding effective oral self care is much more likely to produce the desired result. It can also result in other positive changes, such as giving the patient a greater appreciation for the benefits of comprehensive dental care. If the patient remains unmotivated or is unwilling to modify the circumstances and attitudes that led to the oral problems, then there may be no alternative but to recommend the extraction of questionable teeth and transition the patient to complete dentures. If the patient is receptive and motivated to change, however, then more comprehensive treatment can be suggested. The presentation of treatment options carries unique importance with the motivationally impaired patient. At the outset, such a patient is more likely to have an unusually pessimistic view of the treatment and its chances of success. The same patient may also have unrealistic expectations about how long or how demanding the dental treatment will be. Although candid, the discussion must not be coercive, threatening, or intimidating. Chapter 17 the Motivationally or Financially Impaired Patient 447 the patient must feel comfortable enough with the provider to be able to share what are often deep-seated concerns and reservations. In addition to the usual presentation of treatment options, its risks and benefits, advantages and disadvantages, and the costs in time and money required for each, additional subjective components must be carefully and clearly presented, in particular patient-specific estimation of (1) the likelihood and rewards of success of the treatment and (2) the hazards of failure. Following such an analysis, the patient may be more likely to be engaged in the treatment plan decision making in a meaningful way.
References:
- https://northcarolina.deltadental.com/content/dam/member-companies/north-carolina/form-library/Delta%20Dental%20Dentist%20Handbook.pdf
- https://www.aphl.org/AboutAPHL/publications/Documents/ID_2010May_2009-Viral-Hepatitis-Survey-Report.pdf
- https://pi.lilly.com/us/strattera-pi.pdf
- https://www.easa.europa.eu/sites/default/files/dfu/Easy_Access_Rules_for_Medical_Requirements.pdf